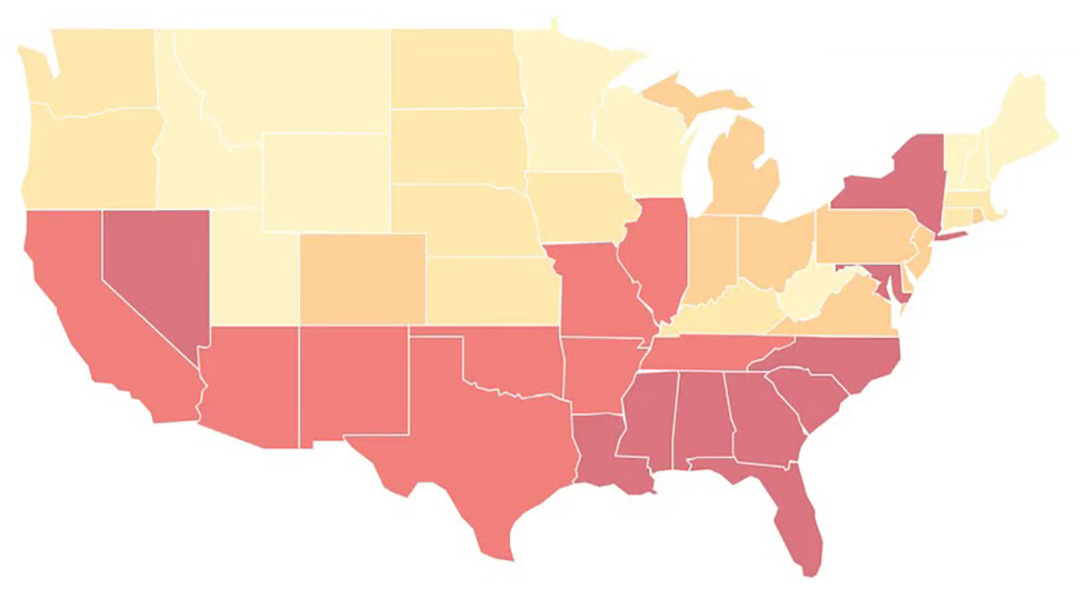
In 2023, South Carolina ranked 6th in the nation in STD rates, as shown by the darker red in the graphic above. The states in yellow have lower rates. (Photo courtesy of Innerbody/Carolina News and Reporter)
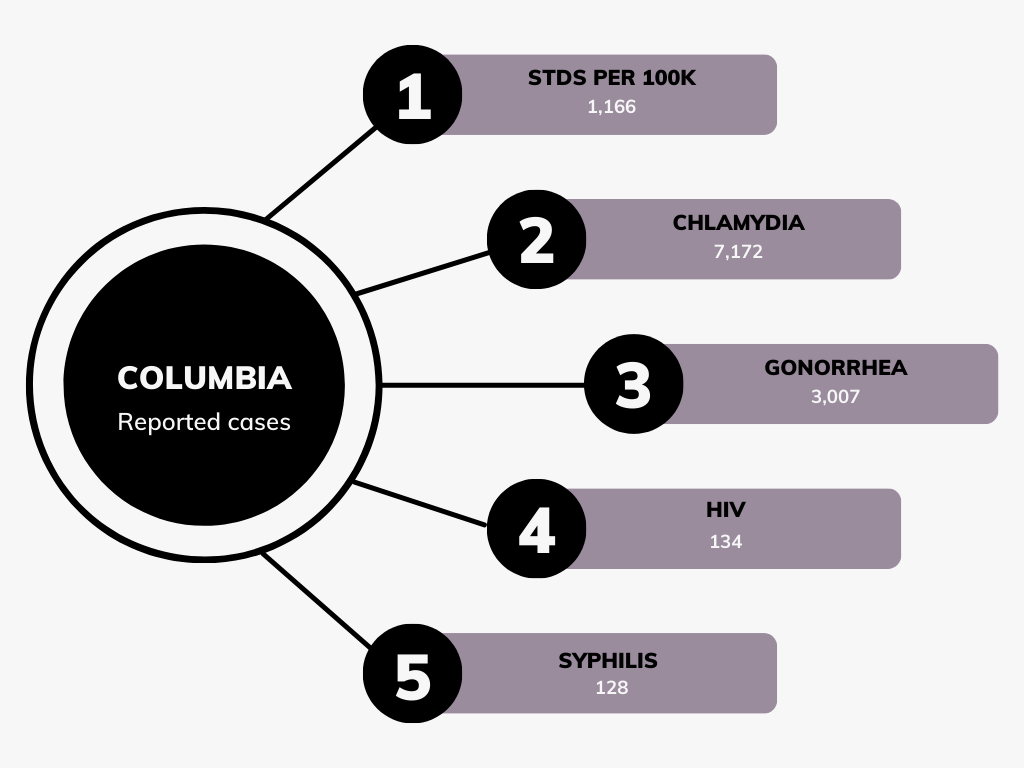
Columbia fell from 3rd to 21 last year among U.S. cities with the highest STD rates, but the drop is likely a result of unreported medical visits, a lack of testing and some people having few to no symptoms.
There were 1,166 cases per 100,000 Columbia residents in 2023, including more than 7,000 cases of chlamydia, 3,007 of gonorrhea and 128 syphilis cases, as reported by Innerbody, an online health research and review site.
South Carolina ranked 6th in the nation in rates of sexually transmitted infections and diseases in 2023.
“South Carolina, we have less cases of gonorrhea and chlamydia being reported,” said Bernard Gilliard, program manager for Partner Services & Disease Intervention with the S.C. Department of Health and Environmental Control.
Gilliard said telecare visits result in more presumptive treatments with fewer lab confirmations for illnesses such as gonorrhea.
Those cases are less likely to be reported to state officials.
“They take them (medication) and they get cured, but they’re never actually documented and counted as cases,” Gilliard said.
Telecare refers to telemedicine and telehealth, which both offer remote medical treatments outside of the in-person doctor-patient connection, according to the Federal Communication Commission’s website.
Telecare offers helpful services for those in need of medical care, but makes it challenging to accurately track the number of people who have STIs or STDs. Patients still obtain treatment, especially those with varying financial status and no health insurance.
But telecare alters the documentation of the sick population. The unreported cases are the problem.
“That’s exactly part of the problem, because we need to be tracking STIs,” said Dr. Helen Stockinger, South Carolina Medical Association president. “It’s always going to be better to have that in person visit.”
Patients must actively get tested to be documented and treated.
The lack of testing can be due to fear of diagnosis or stigma toward these infections.
“‘Well if I go get tested, that’s going to be confirmation, and then I’m going to be thought of, seen or viewed in a particular way,’ and that’s stigmatization,” Gilliard said.
Skipping testing is very dangerous as it increases the risk of cancer and other illnesses, according to the American Society for Microbiology (ASM) website.
“They get over the initial bout, and then late syphilis has neurological complications and cardiac complications,” Stockinger said.
No testing could also be due to the lack of symptoms.
“They’re unaware that they have an STI, unless a specimen was collected in the lab, states that they had an STI or a partner comes to them or somebody, such as a disease intervention specialist comes to them, ” Gilliard said.
These sexually transmitted infections can go without symptoms for days, months or even years, according to the National Health Service website.
Asymptomatic cases are common, according to ASM.
Some people are deceived into thinking they aren’t infected because of mild, cold-like symptoms.
“You don’t recognize it,” Stockinger said. “You just think you’ve got a sore throat. You don’t realize it’s actually a sexually transmitted infection. So these are minor symptoms, and a lot of people think, ‘Well, I just got a cold’… . The symptoms are a little tricky.”
Certain STIs, such as syphilis, are on the rise nationwide, making testing even more important.
The number of instances of congenital syphilis, for example, rose by 937% over the previous 10 years, while cases of syphilis grew by 80% over the previous five years, reported by the Healthline website.
Those rates are the highest in the country since 1950, according to Healthline.
Organizations such as the CDC and Human Health Services are taking measures to decrease the spread of what’s being called an epidemic.
“Ultimately, controlling syphilis and other sexually transmitted infections (STI) require robust public health systems and workforces, and prevention strategies that are tailored to the specific needs of affected communities,” Lisa George, a CDC press officer, said in an email.
Having conversations about these infections and diseases will have an impact on the actual number of cases and ultimately result in a decrease, experts say.
“Normalizing conversation and talk and history extraction about sexual activities … symptoms suggestive of infection – normalizing all of that – plus routinize screening and testing,” Gilliard said.
For those who are affected or in need of testing, organizations such as DHEC offer testing and treatment options.
People need “routinize screening and testing, regardless of age, regardless of any other thing, (like) socio-economic capacity to pay (or) not pay… if they’re engaged in activities that could put them at risk for acquiring a STI, “ Gilliard said.
George said those who are sexually active and/or infected need to make an effort to collaborate with these groups to effectively combat the rising numbers.
“The work and decisions made at the federal level can have a large impact, however turning this epidemic around requires increased ownership of the problem,” George said. “CDC and public funded STI programs cannot do it alone.”
Having conversations about these infections and diseases will have an impact on the number of cases and ultimately result in a decrease. (Photo courtesy of DHEC)
Patients must actively go get tested to be documented and treated, which also affects the number of cases reported. (Photo by Shamariah Vanderhorst/Carolina News and Reporter)