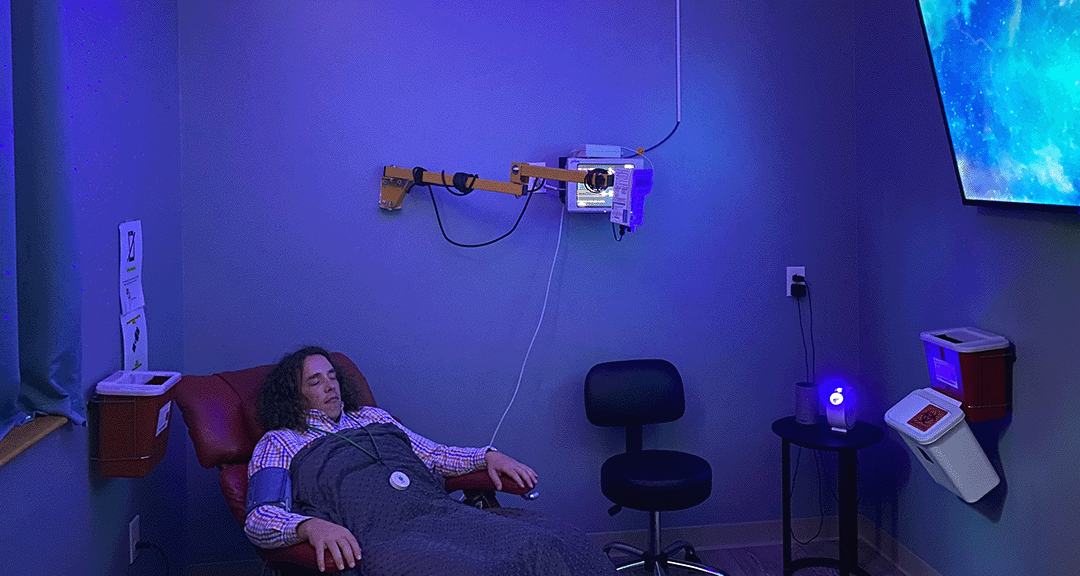
Someone being administered ketamine through an I.V. (Photo courtesy of Charleston Ketamine Center)
“Within 15 minutes of him starting the IV, my (chronic) pain dropped to zero,” said Dawn Gonzales, a ketamine therapy patient from Simpsonville. “I felt the fog start to lift. I was in utter shock. What had I been through?”
Gonzales said she developed a chronic pain disorder two years earlier, after a botched epidural during childbirth. This disorder — called arachnoiditis — causes nerves around the spinal cord to become inflamed.
The pain made it more difficult for the then-33-year-old Gonzales to move on her own.
She said it was difficult to get out of bed to take care of her newborn. She was even having trouble with incontinence.
“I was struggling just to make it through the day with my kids,” Gonzales said. “The burning in my back was getting worse and worse.”
After repeatedly trying various treatments, Gonzales gave ketamine therapy a try. It worked, and the effects lasted for months.
“When I get ketamine infusions, it helps immensely,” Gonzales said. “I can get up more and cook for my family. (I can) travel and sit in a restaurant fairly comfortably. I can still rest without pain. I wasn’t able to rest and sleep more than 30 to 45 minutes at a time for months. I still can’t believe what I’ve been through.”
But it isn’t just chronic pain treatment. Patients and doctors in South Carolina say they are also having success using ketamine therapy to treat mental illness.
Ketamine therapy for the mentally ill is a form of clinical therapy in which patients are given a ketamine infusion, then undergo a counseling session with a doctor.
“Ketamine is a dissociated anesthetic that has been used for years and years in surgery,” said physician David Smith, a practitioner at Tidewater Health and Ketamine Center. “They noticed people were coming out of surgery feeling better, so they started to do research on it.”
WHAT IT IS
Ketamine can be administered through pills, IV or nasal spray. Ketamine given as a prescription is typically a lower dose than what you would receive at a clinic, according to medical researcher and physician Richard Bowen, who practices at the Charleston Ketamine Center.
Ketamine is in a category of drugs described as “ineffable,” according to psychiatrist Juan Pablo Galindo, a practitioner at Innerbloom Healing Arts in Charleston. These types of drugs, usually psychedelics, are labeled ineffable because their effects are individualized and difficult to describe. Researchers haven’t yet figured out why they work — only that they work.
“We are not sure why it makes people with chronic pain better,” Bowen said. “People think it is possible that it changes the brain’s interpretation of the pain, or it even increases the (brain’s) pain threshold.”
But Michael Leach, a certified medical assistant at the organization Addicted — also known as Drug Rehab Services — notes the potential addictive qualities of the drug.
“The primary dangers are its dissociative effects, causing a person to feel detached from their body and causing visual and auditory hallucinations,” Leach said. “The prolonged use of ketamine leads to addiction, tolerance and dependence.”
With ketamine therapy clinics being relatively new — the first in the United States opened in 2015 — it is difficult to tell what the long-term effects of the treatment could be.
A 2021 study conducted by members of the Royal College of Psychiatrists in London found large doses of ketamine can cause schizophreniform symptoms — a temporary form of schizophrenia that can last for months.
But the addictive potential of ketamine is low in a controlled medical setting, Bowen said.
“We can get addicted to anything — drugs, sex, or gambling,” he said. But “we don’t get physically addicted to things like gambling. The same is true for ketamine.”
Ketamine, Bowen said, can cause people to get addicted to the psychological effects, whereas heroin is a drug where people can get physiologically addicted — meaning users feel physical symptoms during withdrawal.
It’s too early to tell if addiction is a significant side effect.
HOW IT WORKS
As of this year, there are almost 600 private ketamine clinics across the country.
Ketamine therapy, as the name suggests, is ketamine and therapy mixed together. In short, the two can’t be separated.
Ketamine is administered to the patient, who is relaxing in a comfortable chair, through an IV. Some practitioners will have patients wear sleep masks or headphones.
“After about 15 minutes, the patient starts to feel the effects of the drug,” Bowen said. “The effects last for about 40 minutes. But once you take the IV out, it takes about 15 minutes before the patient is fully back” from the anesthetic feel of the drug.
In the psychedelic therapy community, there is a phenomenon called the Window of Tolerance, Galindo, the psychiatrist, said. The Window of Tolerance model is split into three parts: hyper-arousal, the window of tolerance and hypo-arousal.
Hyper-arousal is when a person is too high energy or angry to effectively respond to therapy. Hypo-arousal is when a person is too low energy or anxious to effectively respond to therapy. The window of tolerance is the “in-between” where therapists want their patients to be.
“The window of tolerance is a common term associated with psychedelics,” Galindo said. “Ketamine widens this window of tolerance so people can engage in therapy without getting overwhelmed.”
Patients start the talk-therapy portion of the treatment while ketamine is still in effect. Doing so can help patients feel more comfortable saying things they wouldn’t normally share, Bowen said.
The majority of each clinic’s patients are being treated for some sort of depression, anxiety or PTSD. Ketamine therapy starts with four to six infusions within the first week. Patients normally begin to feel the effects between the fourth and sixth infusions.
Ketamine can reduce moderate to severe depression by up to 70%, according to the Charleston Ketamine Center’s study of its own patients.
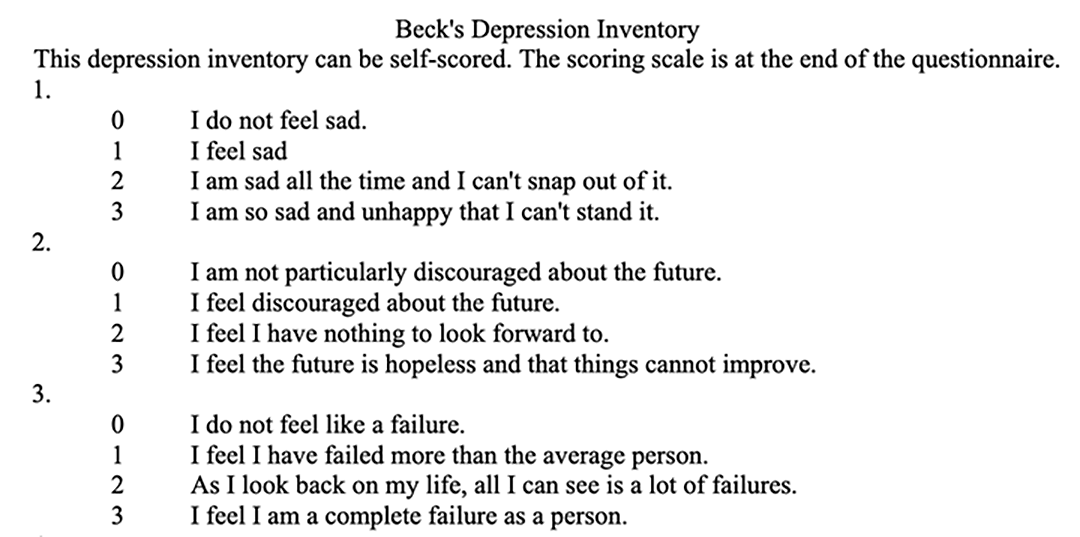
The center uses the Beck Depression Inventory on each patient’s visit to track long-term improvement and aid in the clinic’s own research.
The effects of a single ketamine treatment can last months, Bowen said.
But Wesley Ryan, an addiction psychiatrist, worries the proliferation of clinics can get ahead of science and regulations.
“A not insignificant minority of clinics offer ‘package deals’ on ketamine, grossly misrepresent the treatment by suggesting it is a ‘cure’ for depression or make unsubstantiated and exaggerated claims about efficacy,” said Ryan said, without commenting specifically on Charleston Ketamine Center’s data.
HOW WE GOT HERE
In the early 1970s, the Nixon administration declared a “War on Drugs.” The goal of this “war” was to reduce the illegal drug flow into the United States. The administration created a drug schedule to rate a drug’s medical usefulness and potential for abuse. That’s when the Drug Enforcement Administration was formed.
These policies, put in place nearly half a century ago, still make it difficult for scientists and doctors to research illegal substances. The DEA delineates drugs as being in one of five categories. Schedule I drugs are considered highly addictive with little medical value, while Schedule V drugs — such as cough syrup — are considered medically useful and non-addictive.
Heroin, LSD, and marijuana are Schedule I drugs, which makes them difficult for researchers to study.
“I would love to use LSD or psilocybin (a chemical in “magic mushrooms”), and I anticipate it will be used soon,” Bowen said.
For comparison, cocaine is a Schedule II drug, while ketamine is a Schedule III drug. Schedule III drugs show moderate to low addictivity but have a potential medical use, which allows doctors and pharmacists to legally handle the drug. Restrictions vary by state.
However, working with medications on the drug schedule list can be expensive for patients, even if they get clearance for therapy. Insurance companies are wary about covering the cost of therapy using these drugs, especially if there are other medications available.
“It would take a lot of lobbying or class action (lawsuits) to get insurance companies to cover more,” Bowen said.
A single three-hour session can cost between $500 to $1,000, Galindo said.
Gonzales wishes that ketamine was more accessible, especially for those who suffer from chronic pain as she does.
“Sadly, it is very expensive — and quite often, not covered by insurance in an outpatient setting,” Gonzales said. “So I have to go without (ketamine therapy) most of the time.”