A harm reduction volunteer at Challenges Inc., Kris Stepp, helps someone test her drug supply for xylazine. (Photo by Eva Flowe/Carolina News and Reporter)
Lala Littleton tests her drugs before she takes them. For about the last year, her heroin, meth and fentanyl have regularly been testing positive for the veterinary tranquilizer xylazine.
But she’s never once sought out the drug.
The sedative is often used to “cut” other substances, particularly opioids. The drug, legally used to tranquilize large animals, can cause large open wounds on people’s bodies.
Littleton, a 33-year-old living outside Greer, has a mark on her upper-arm consistent with a healed xylazine wound. She has had it a couple of months, when her supply started testing positive.
“It started being in the dope that I was getting (so often), to the point where I don’t even talk to the person I get it from about it,” Littleton said. “Now it’s in all of it.”
Xylazine is used to cut opioids because it is inexpensive, unregulated and can allow drug traffickers to reduce the amount of heroin or opioids they use, because it can make the effects of opioids feel stronger to unsuspecting users, according to the U.S. Drug Enforcement Agency.
South Carolina health officials are still grappling with just how prevalent the drug is, but in the meantime, lawmakers are pushing for harsher penalties for users and sellers.
Littleton said she’s thankful her wound never got bigger, because she has seen what untreated xylazine wounds can be: Large patches of rotten and blackened skin covered in pus that takes a long time to heal.
When she started visiting a mobile harm-reduction unit in Greenville to get clean syringes three years ago, she had never heard of xylazine. It primarily had been found in illicit drugs in the Northeast, especially in and around Philadelphia.
The Upstate-based Challenges Inc. distributes syringes and naloxone, an anti-overdose drug for opioids often called by its brand name, Narcan, to people struggling with drug abuse in South Carolina. The organization also provides fentanyl and xylazine test strips, which is what Littleton uses to test her drugs.
Marc Burrows, the executive director, said xylazine is in South Carolina, but it’s hard to know just how much is being mixed into other drugs because neither the state nor hospitals test consistently for xylazine.
South Carolina Sens. Danny Verdin, R-Laurens, and Sandy Senn, R-Charleston, have introduced a bill to make it a felony to manufacture or sell xylazine for human use.
The bill passed the Senate unanimously April 3. A companion bill is in the S.C. House of Representatives. It might not pass this year but could be reintroduced next year.
“I put the bill forward because xylazine is probably the scariest drug I’ve ever even heard of, and it certainly will be the most lethal and cheap in our state,” Senn told the Carolina News and Reporter. “I am very worried that young people who are already exposed to fentanyl will now also be exposed to this big animal tranquilizer.”
The bill was amended to exclude veterinarians from prosecution, as they may need xylazine to operate.
Marie Queen, executive director of the South Carolina Association of Veterinarians, said it was important that veterinarians be excluded.
“The xylazine that’s being trafficked or diverted is not the same one that’s used in veterinary hospitals,” Queen said.
She said the organization worked with the state Department of Health and Environmental Control to help advance the bill and advocate for veterinarians.
A DHEC public health order released in November requires healthcare practitioners to report when toxicology lab results are positive for xylazine.
DHEC shared data on fatal overdoses involving xylazine with the state Legislature this year. That doesn’t inherently mean xylazine caused the overdoses, as opioids are almost always present.
South Carolina in 2021 documented 91 fatal overdoses in which xylazine was found. DHEC’s provisional data documented 177 cases in 2022, and 100 in 2023.
Nabarun Dasgupta, a scientist who tests drugs at the University of North Carolina at Chapel Hill, said his lab has received 18 drug samples from South Carolina in the past three years, and only one contained xylazine.
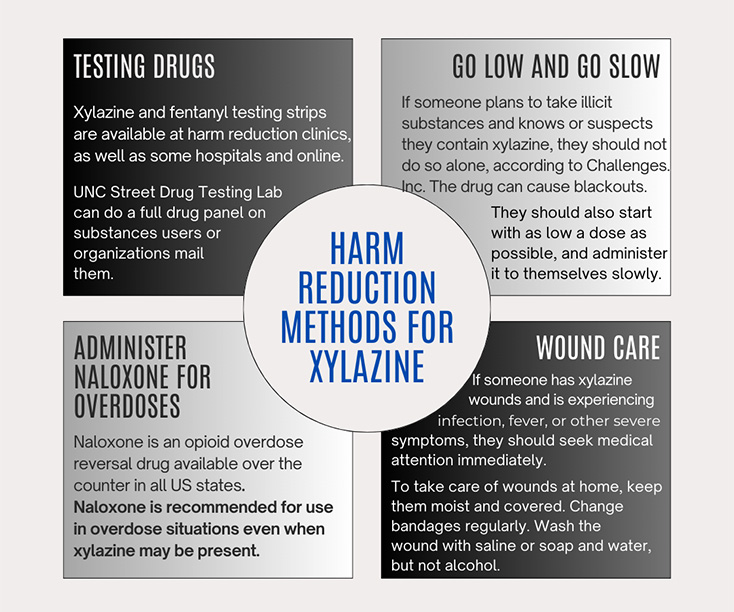
The CDC contends Naloxone does not reverse the effects of xylazine but still recommends use of the antidote on people who have xylazine in their systems, because other opioids are often involved.
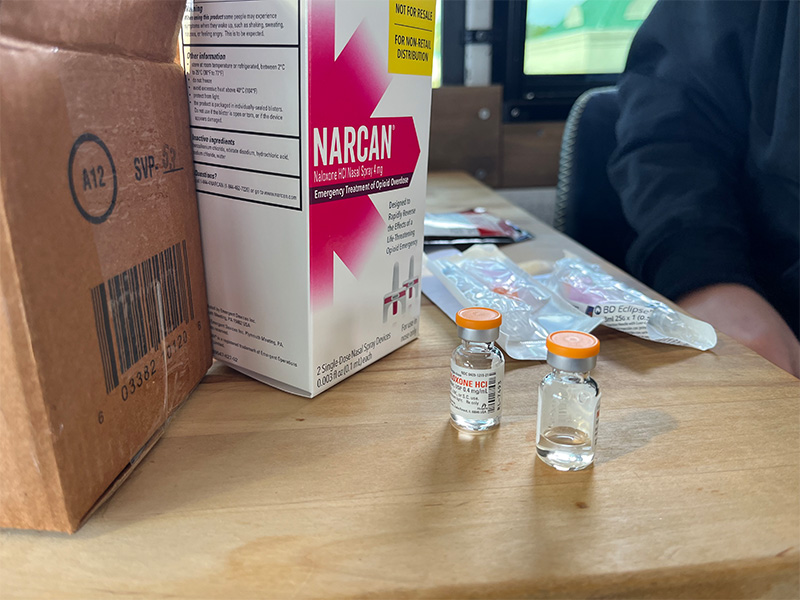
Dasgupta said some new research has shown that naloxone is actually effective against xylazine. But people who have overdosed on other opioids could be slower to awaken after Naloxone is administered if they have xylazine in their system.
This can be a problem at times, because the user sometimes has been injected with too much naloxone, sending them into severe withdrawal, Dasgupta said.
Xylazine withdrawal also differs from the withdrawal from traditional opioids. It can last longer and involve more anxiety and agitation.
One of the scariest developments in the drug’s introduction to the market has been unnecessary amputations, Dasgupta said.
When xylazine wounds first started appearing on patients’ arms in North Carolina, that’s when the amputations began at hospitals, Dasgupta said. The wounds looked atypical, and doctors knew they needed to treat them differently than normal injection-site wounds. His team at UNC stopped two amputations.
“People were literally getting their arms and legs cut off when they didn’t need to be,” Dasgupta said. “A lot of folks around the state kind of stepped up and pointed out that these are wounds that heal more like a chemical burn.”
The wounds do not necessarily show up at injection sites. They are often on the arms and legs, but have been seen elsewhere, including in the nasal cavity. They are sometimes necrotic, or rotting.
Dr. Poornema Ramasamy is a wound care physician at Prisma Health in Columbia who volunteers doing wound care for people struggling with substance abuse disorders. She said she hasn’t seen xylazine wounds volunteering, but she has seen a few suspicious wounds at the clinic where she works.
But the people who had possible xylazine wounds rarely returned, often because of transportation and insurance issues, Ramasamy said.
“I’ve brought people into the hospital, and had nurses and doctors come by and marvel at them,” Dasgupta said. “Because these wounds were so different and horrific, they made them feel like a medical oddity.”
South Carolina officials hope the state doesn’t face an influx of drug users dealing with effects of xylazine. But making it a felony could come with some risks. Rollie Martinson, a volunteer harm reduction specialist with Challenges, said one potential consequence could be that drug sellers instead cut drugs with something more potent.
The House bill is in the Committee on Medical, Military, Public and Municipal Affairs, where it’s been since April 9.
(Graphic by Eva Flowe/from Nabarun Dasgupta, Kris Stepp, Rollie Martinson/Carolina News and Reporter)
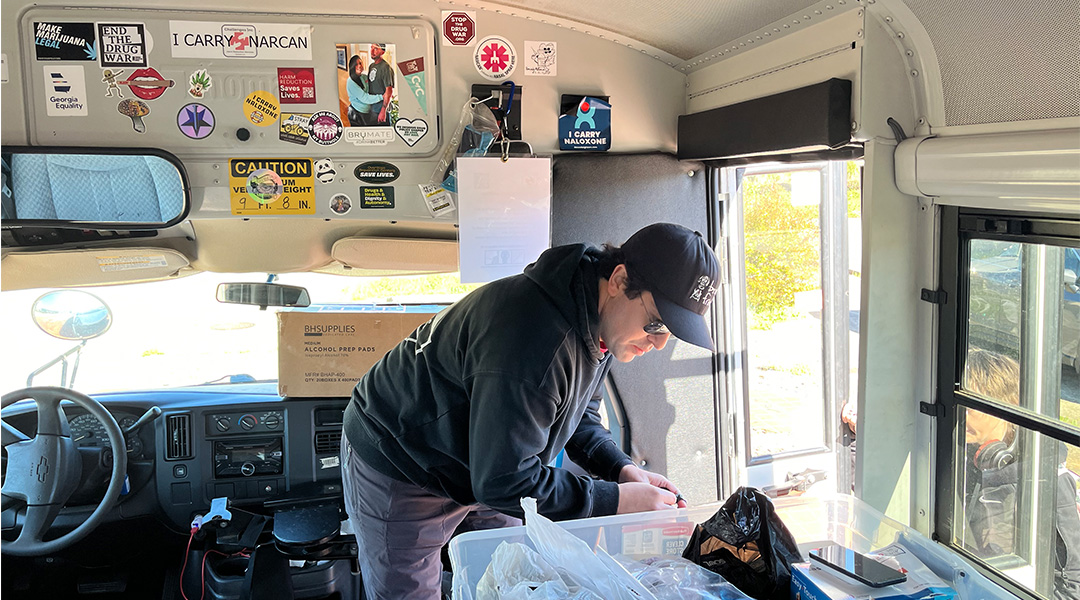
Rollie Martinson, a volunteer harm reduction specialist, hands out syringes and naloxone from the mobile unit of Challenges Inc. in Greenville. (Photo by Eva Flowe/Carolina News and Reporter)
Bottles of intravenous naloxone. Martinson said people addicted to drugs often prefer injectable naloxone because it comes in a smaller dose and therefore does not cause as intense a withdrawal. (Photo by Eva Flowe/Carolina News and Reporter)
Someone on the Challenges Inc. bus prepares to test their drugs for fentanyl and xylazine. (Photo by Eva Flowe/Carolina News and Reporter)